No, the GOLO Release supplement, which includes 210 mcg of chromium, as supported by two separate studies conducted in 2021, does not raise blood pressure (hypertension). In fact, these studies indicate that chromium supplementation can have a positive impact on blood pressure.
A study by Omid Asbaghi from Shahid Beheshti University of Medical Sciences found that chromium supplementation significantly reduced diastolic blood pressure by -2.36 mmHg and malondialdehyde levels. However, it did not significantly affect systolic blood pressure or other parameters like body mass index or liver function enzymes.
On the other hand, another study by Abolfazl Lari from Iran University of Medical Sciences conducted a systematic review and meta-analysis of randomized clinical trials. This analysis also showed a significant decrease in both systolic blood pressure by -2.51 mmHg and diastolic blood pressure by -1.04 mmHg following chromium supplementation.
Hypertension, as defined by the 2018 study by Suzanne Oparil from The University of Alabama at Birmingham, is a systemic arterial condition characterized by elevated and persistently high blood pressure. It is a major modifiable risk factor for various health issues, particularly cardiovascular disease, and can result from a combination of genetic predisposition and environmental factors.
So, does the GOLO diet cause high blood pressure? No, the 2000 study by K Hermansen titled “Diet, Blood Pressure, and Hypertension” highlights the role of lifestyle modifications, including weight loss, in effectively lowering blood pressure. Even a modest weight loss of 3-9% is associated with a significant reduction in both systolic and diastolic blood pressure, especially in overweight individuals. However, it’s important to note that dietary factors, such as sodium intake, also play a role in blood pressure regulation.
This article explores the effects of the GOLO diet on blood pressure and examines the interactions with the most common medications.
What are the causes of hypertension?
Hypertension, as described by Suzanne Oparil, a clinical cardiologist and distinguished Professor of Medicine, is a medical condition characterized by persistently high blood pressure in the systemic arteries. It is a major risk factor for cardiovascular disease and can lead to serious health complications if left untreated.
The causes of hypertension are multifactorial and involve a combination of environmental and pathophysiological factors, as well as genetic predisposition. Factors such as sodium consumption, obesity, physical inactivity, aging, and genetic variations can contribute to the development of hypertension.
- High salt intake: Excessive consumption of sodium can lead to fluid retention and increased blood volume, contributing to high blood pressure. A 2017 study by Wenguang Feng from Veterans Affairs Medical Center has shown that a high salt intake of more than 5 grams per day is associated with a 23% increased risk of developing hypertension. Reducing salt intake to less than 2 grams per day has been found to lower blood pressure by an average of 4-5 mmHg.
- Obesity: Being overweight or obese significantly increases the risk of hypertension, with one 2018 study published in Nature Reviews Disease Primers Journal showing that individuals who are overweight have a 22% higher risk of developing hypertension compared to those of normal weight. Furthermore, multiple studies, including the Nurse’s Health Study and the Framingham Heart Study, have demonstrated a strong association between increased body mass index and the development of hypertension.
- Sedentary Lifestyle: A sedentary lifestyle, characterized by a lack of physical activity, significantly increases the risk of weight gain and the development of hypertension. As supported by a 2015 study conducted by Larissa Castelo Guedes Martins from Universidade Federal do Ceará, a sedentary lifestyle is prevalent, with 55.8% of patients with hypertension exhibiting this diagnosis. Additionally, exposure to acute prolonged uninterrupted sitting has been shown to result in significant increases in systolic blood pressure and mean arterial pressure, particularly in younger age groups.
- Alcohol Consumption: According to a 2006 study by Ian B. Puddey from the University of Western Australia, regular alcohol consumption is associated with an elevation in blood pressure, contributing to a 16% attributable risk for hypertensive disease globally. For every 10 grams of alcohol consumed, blood pressure increases by approximately 1 mmHg, but this effect is largely reversible within 2-4 weeks of abstinence or a significant reduction in alcohol intake. The increase in blood pressure is consistent across different types of alcoholic beverages, and the postulated effects of vasodilator flavonoid components in red wine to mitigate alcohol-related hypertension have not been supported by intervention studies.
- Genetic Factors: Genetics plays a complex role in hypertension, with multiple genes contributing to blood pressure regulation. A 2010 study by Merlin G Butler from Kansas University Medical Center suggests that genetics accounts for 30%-50% of blood pressure variance, while environmental factors make up the remaining 50%. Specific genes related to sodium handling, the renin-angiotensin-aldosterone system, hormonal regulation, and vascular tone have been implicated in blood pressure regulation.
Based on the available scientific evidence and the principles of the GOLO diet, it is unlikely that the GOLO diet would raise blood pressure. In fact, the diet is designed to address factors that can contribute to high blood pressure and promote overall cardiovascular health.
What is the effect of the GOLO diet on blood pressure?
The effect of the GOLO diet on blood pressure was evaluated in a study by Robert J. Buynak in 2019. The study included 68 subjects with an average baseline weight of 106.97 kg and an average BMI of 38.82 kg/m², which is considered obese.
The results of the study showed that subjects randomized to the GOLO diet supplement (treatment group) experienced significant improvements in their blood pressure compared to those assigned to the placebo group. Specifically, diastolic blood pressure in the treatment group decreased by an average of -4.11 mmHg, while the placebo group showed a smaller increase of 1.31 mmHg, as shown in this diagram.
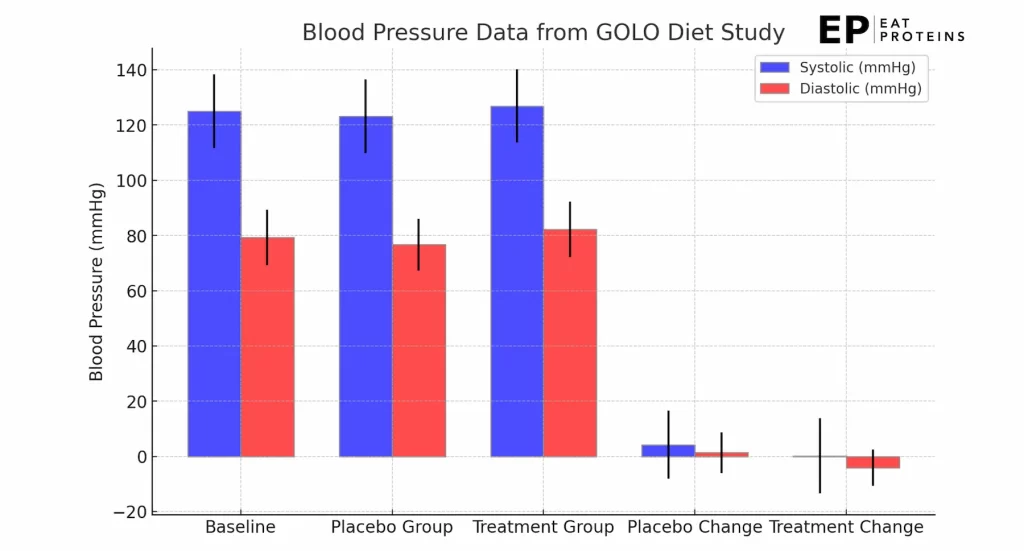
This reduction in diastolic blood pressure in the treatment group was statistically significant. Additionally, the treatment group exhibited a statistically significant decrease in pulse rate, with an average reduction of -3.44 bpm, compared to a 4.38 bpm increase in the placebo group. These changes in vital signs indicate that the GOLO diet may have a positive effect on blood pressure and heart rate.
How does the GOLO diet impact the use of blood pressure medication?
The impact of the GOLO diet on the use of blood pressure medication is substantial. In a 2021 study by Wilma S Leslie from the University of Glasgow involving 143 participants, 78 of whom were initially on hypertension treatment, the mean blood pressure significantly decreased during the total diet replacement phase.
Of those previously on hypertension treatment, 83% were able to discontinue all antihypertensive and diuretic medications as per the protocol. Additionally, 28% of participants remained off medications at 24 months, even after achieving sustained diabetes remission with a mean weight loss of 11.4 kg.
However, reintroduction of antihypertensive medications was necessary for some participants, particularly those previously on two or more drugs, with approximately 27.5% requiring medication reintroduction during the total diet replacement. Mild to moderate dizziness was reported, particularly among those with prior dizziness and those on antihypertensive or diuretic medications.
Does the GOLO diet interact with common medications?
Yes, the GOLO diet, which includes 210 mcg of chromium as a main ingredient, can interact with common medications, particularly biguanides like metformin. Chromium is known to influence insulin resistance and can lower blood sugar levels. When considering taking GOLO with metformin, there is a potential for hypoglycemia (low blood sugar). Therefore, it’s crucial to consult a healthcare provider and have the combination supervised, especially if you have diabetes or other related conditions.
